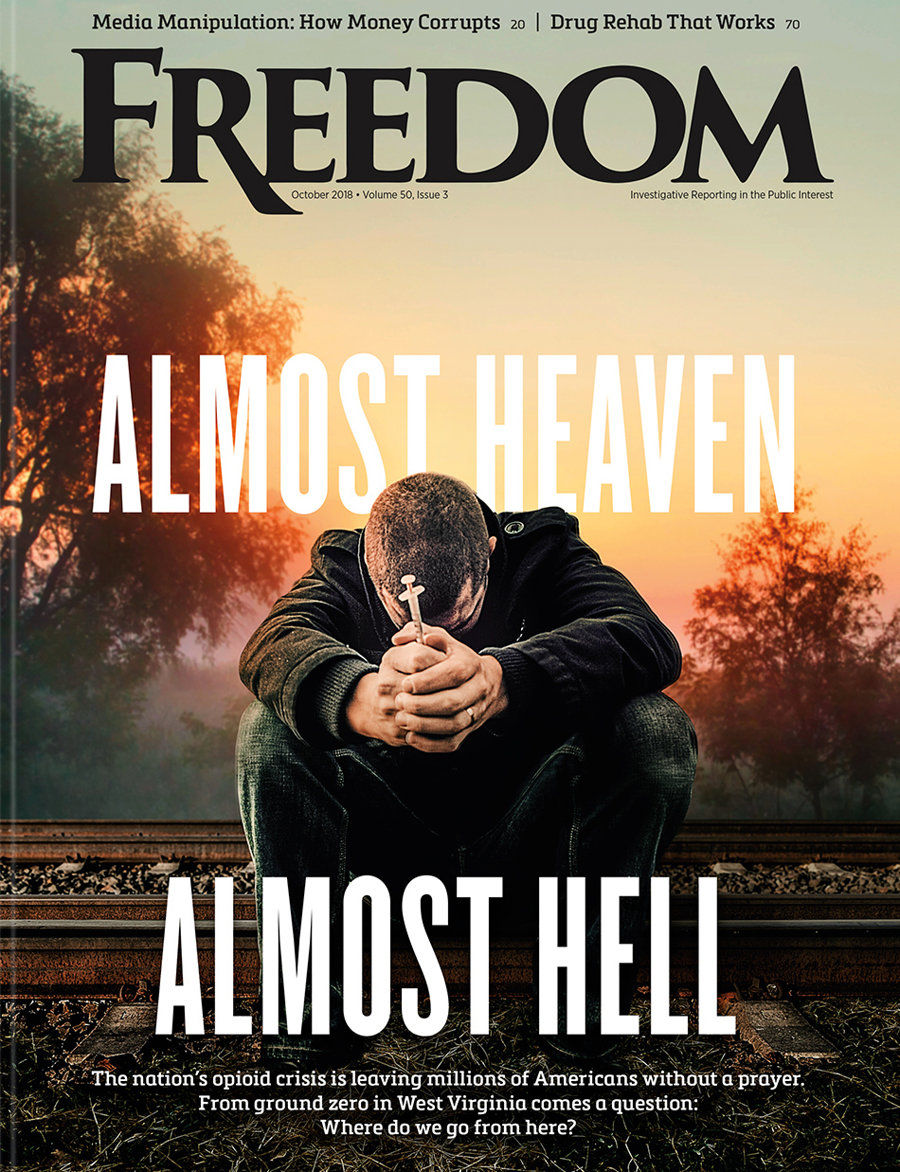
Fifty to 100 times more potent than morphine, fentanyl can be combined with drugs like cocaine and heroin or added to other substances to enhance their strength. Even a small dose of fentanyl can be lethal, so it is little wonder that the narcotic contributes to the bulk of all drug overdose deaths. In 2021 alone, nearly 71,000 of the more than 107,000 US overdose deaths involved synthetic opioids according to Addiction Group, a public information portal where scholars and medical professionals write about current scientific research.
According to the Health Resources and Services Administration’s most recent overview of the opioid crisis, updated in December 2023, more than 130 people in the US lose their lives each day due to opioid overdoses.
A partnership between Stanford University and the esteemed British medical journal Lancet, the Stanford-Lancet Commission on the North American Opioid Crisis predicts that opioid deaths (which are already eight times higher than in 1999, when the first wave of deaths involving prescription opioids unleashed the crisis) will reach an additional 1.2 million nationwide by 2029 if no new measures are implemented to combat the epidemic. Additionally, polysubstance use—where fentanyl is combined with other drugs like cocaine or alcohol—further increases the risk of fatal overdoses.
The FDA is effectively using its nearly $3 billion annual drug budget to approve more medications just like those that fueled the opioid crisis in the first place.
Current efforts to address the crisis focus on increasing “harm-reduction” services, such as the distribution of naloxone—a medication that counteracts the effects of opioid overdoses—and improving addiction treatment infrastructure. But more reforms are clearly needed to tackle the root causes and regulatory failures that fueled what the Stanford-Lancet Commission describes as one of the most devastating public health disasters of the 21st century.
The FDA’s role in aggravating the opioid crisis is notorious. The agency approved powerful prescription opioids like OxyContin, manufactured by Purdue Pharma and first sold in 1996, for long-term use, despite limited evidence of their safety for chronic pain management.

In fact, the overprescription of OxyContin occurred during the most heavily funded promotional campaign in the history of pharmaceuticals, the Stanford-Lancet Commission notes, adding that the result was a fourfold increase in opioid prescriptions. And all the while, Purdue Pharma downplayed the addictive risks of the drugs, leading physicians to prescribe them more liberally.
OxyContin alone is estimated to have brought in over $35 billion in revenue for Purdue Pharma and its owners, the Sackler family.
On June 27, 2024, a court overturned the 2021 bankruptcy settlement for Purdue Pharma and the Sackler family, citing that the agreement breached US bankruptcy law by absolving the Sacklers of liability without the consent of the claimants. Despite this, Purdue Pharma remains operational.
The latest development in the ongoing opioid epidemic reveals a change in the government’s language, as it reclassifies the calamity as an “overdose crisis,” thereby placing more emphasis on overdose deaths than on opioid misuse itself. In line with this change, drugs like Narcan and other post-overdose treatments are being released, including a new medication released by Purdue Pharma this past August.
In 2022, the FDA introduced an “Overdose Prevention Framework,” detailing four main priorities. The first focused on preventing unnecessary initial exposure to prescription drugs and limiting inappropriate long-term prescribing practices. The second aimed to promote harm reduction through innovative strategies and public education. The third and fourth goals were to support the development of evidence-based treatments for substance use disorders and to safeguard the public from unapproved, diverted or counterfeit drugs that pose overdose risks.
Eight of the experts had financial connections to pharmaceutical companies, including Purdue, and they advised the FDA against limiting the indication for opioids.
Yet the FDA and other key players in the opioid crisis seem to falter in two primary ways: First, their emphasis on overdose prevention—through measures like over-the-counter Narcan—tends to overlook crucial root causes of overdoses, including addiction and the illicit drug trade. Second, rather than addressing these deeper issues, they continue to seek pharmaceutical fixes, developing alternative painkillers or modifying existing drugs to reduce their potential for abuse.
The FDA is effectively using its nearly $3 billion annual drug budget to approve more medications just like those that fueled the opioid crisis in the first place, while also greenlighting treatments designed to revive individuals after they overdose on the very opioids the agency already sanctioned.
It’s useful to recall that, in 2017, the President’s Commission on Combating Drug Addiction and the Opioid Crisis determined that inadequate oversight by the FDA was partly responsible for the opioid epidemic. The National Academy of Sciences also publicly urged the FDA to reform its opioid policies. And in 2019, a former FDA commissioner criticized the agency on 60 Minutes, stating that it was a mistake to permit the promotion of opioid use for chronic pain.

Despite the mounting criticism, FDA policies for approving and labeling opioids remain largely unchanged, according to an August 2020 article in the AMA Journal of Ethics. Authored by Andrew Kolodny, medical director of the Opioid Policy Research Collaborative at Brandeis University, the article noted that the FDA has not undertaken a root-cause analysis of its regulatory errors that contributed to this public health catastrophe, let alone instituted any major reforms.
To the contrary, the agency has adopted a defensive posture and sought to shift blame. For example, in response to a critical letter from Senator Maggie Hassan of New Hampshire, the FDA’s top official at the Center for Drug Evaluation and Research offered a blanket defense of the federal agency’s handling of opioids, claiming that the FDA has properly enforced the Food, Drug and Cosmetic Act.
Moreover, large pharmaceutical distributors, including McKesson, AmerisourceBergen and Cardinal Health, shipped massive amounts of opioids to pharmacies across the US, often targeting small communities where addiction and overdose rates subsequently soared. These companies failed to fulfill their legal obligation to report suspicious orders of opioids, contributing to the worsening public health crisis.
In response to evidence that opioid prescriptions had exceeded clinically justified levels, the FDA called an advisory committee meeting with 10 external experts all the way back in 2002. They discussed whether the broad indications on opioid labels should be restricted.
Eight of the experts had financial connections to pharmaceutical companies, including Purdue, and they advised the FDA against limiting the indication for opioids. This missed opportunity to curb overprescribing early in the crisis led to a situation where, by 2013, there were enough opioids prescribed to supply every adult in the country with a full bottle of pills.
“Oversight bodies within the Executive Branch and Congress should conduct a long-overdue examination of the FDA’s role in the opioid crisis,” wrote Kolodny in his AMA Journal of Ethics article. “Understanding why our regulatory systems failed to prevent a man-made epidemic is a critical step toward abating the opioid crisis and preventing future public health catastrophes.”